Newsroom
Welcome to our newsroom, where you can find the latest news about our Trust.
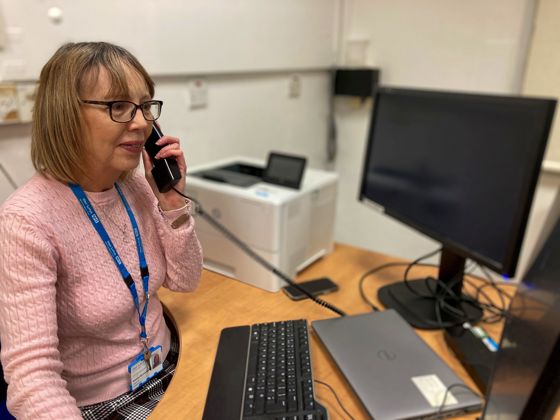
Ros has been on the line for 30 years
Trust news
CEO Column – November 2025
Trust news

Two executive appointments confirmed
Trust news

My WiSH Charity celebrates 30 years
Charity news

Take your medication on time, every time
Trust news